About…
Archives: Advocacy
AAP Global Climate Change and Children’s Health Resources
AAP Resources, Policy Statements, Technical Reports
Climate Advocacy Skill-Up for Health Professionals
This video is a training, organized by Climate Health Now, which includes an overview of California’s climate policy, a powerful storytelling workshop, and a discussion with leading climate and health advocates on how health professionals in California can support ambitious climate action.
Take Action
Find community for climate advocacy by joining our Task Force! Also consider joining state-wide organizations such as Climate Health Now, and national organizations like the Health Care Without Harm Physician Network, and Physicians for Social Responsibility (PSR) for additional learning and advocacy opportunities.
Provide More Resources for Patients-INACTIVE Mental Health Issue
Resources for Families
[ More Coordinated website would be helpful! __]
Talking to Families About Mental Health:
What questions to ask patients and families to update on mental health issues
http://pediatrics.aappublications.org/content/pediatrics/125/Supplement_3/S159.full.pdf
[This resource is helpful but not the best as the first one listed__]
Helping Your Child Cope with Anxiety
http://www.ohioaap.org/wp-content/uploads/2013/07/Helping-Your-Child-Cope-with-Anxiety.pdf
Facts for Families Guide – Table of Contents
Listing of general information that pediatricians can easily refer patients to:
National Alliance on Mental Illness (NAMI)
https://nami.org/Support-Education
-This website also has some information in Spanish and link to regional chapters: NAMI California
Sesame Street
[___]
See also COVID resources
Improve Your Practice – Mental Health Skills and Practice Management
Whether you’re looking for a book, webinar, or mini-fellowship, the first section on this page walks you through the range of general educational tools to help you build your skills on mental health care for your patients and families.
This section includes:
- General Tools on Improving Your Mental Health Skills
- Identifying Pediatric Mental Health Concerns in your Practice
- Course, Trainings, and Fellowships
- Mental Health Integrated Care and Telepsychiatry
General Tools on Improving Your Mental Health Skills
-
AAP Mental Health Initiatives Primary Care Tools
- This is the potentially most useful AAP site that contains all of the tools created by the AAP Task Force on Mental Health; if you go through each of the bulleted list, you can find information that can be helpful to you and your practice.
-
AAP Mental Health Initiatives – Implementing Mental Health Priorities in Practice
- This website includes videos that can be helpful for the primary care practitioner in terms of learning new approaches and also different ways to address common mental health and behavioral problems.
-
Mental Health Competencies for Pediatric Practice
- 2019 article by Jane Foy and AAP COPACFH which describe brief interventions and other skills helpful for pediatricians to use regularly. It stresses the “common factors approach” and re-introduces the HELP mnemonic. It has something for the practitioners and also something for the practice.
-
Pediatric Mental Health Minute Series
- Quick, yet in-depth videos on core pediatric mental health concerns aim to improve your knowledge and skills and support you in caring for children and youth with mental health disorders. Topics include Antidepressants, Suicide, Adolescent Depression, Trauma Informed Care and Anxiety.
-
Additional books of interest
-
Mental Health Care of Children and Adolescents: A Guide for Primary Care Clinicians. By Foy, Jane M ed., American Academy of Pediatrics. 2018
- This book was produced through the efforts of many contributors, many of whom served on the AAP Mental Health Leadership Workgroup. It outlines topics such as “The Pediatric Advantage”, “Enhancing Pediatric Mental Health Care” and gives a lot of algorithms and practical ideas on how to address pediatric mental health and behavioral health issues in the primary care office.
-
Promoting Mental health in Children and Adolescents: Primary Care Practice and Advocacy. By Foy, Jane M ed., American Academy of Pediatrics. 2019.
- This book aims to help pediatric primary care clinicians to integrate anticipatory guidance on healthy social-emotional development into their practice, identify emerging symptoms of mental health disorders and apply brief evidence-based interventions to the care of children with mental health risks and problems.
-
Identifying Pediatric Mental Health Concerns in your Practice

Pediatricians and primary care providers have long recognized that most mental health issues begin in childhood. Pediatricians have a unique role in identifying children and assisting families early in the evolution of mental health concerns. The symptoms presenting in the office setting are often within the context of a new “problem” or ongoing behavioral concern. The pediatrician’s role is to work with the family to identify whether or not the targeted behavior is a normal variant for age and whether it seems to be impacting the child’s or family’s daily life and/or developmental progress.
For information on identifying and managing specific mental health disorders:
-
The Presentation of Mental Health disorders in the Pediatric Office
- This is a description of the most common pediatric concerns seen in your practice and their presentations.
-
Using your present office screens and skills to identify concerns
- Many of the screens that you are presently using in your practice can facilitate identifying pediatric mental health disorders. Additional screens are available on-line through the AAP Screening Technical Assistance & Resource Center (STAR Center).
- Surveillance, Screening and Psychosocial Assessment for Behavioral Health Concerns
- For more information on Surveillance and Screening particularly for psychosocial/behavioral assessments, developmental delay, and maternal depression.
-
Anxiety
-
Depression and Suicide
-
Behavioral Concerns such as Problems with Attention, Emotional Dysregulation and Aggression
Courses, Trainings and Fellowships
-
AAP ECHO Trauma and Resilience Course
- This is an interactive, case-based, online two-level curriculum program for health care professionals to learn about and improve the identification, care, management and outcomes of traumatized children and their families in pediatric settings. CME and MOU credits are available for participation.
-
REACH Institute
- The REACH Institute offers a “mini-fellowship”; in pediatric psychiatry for general pediatricians called “Patient Centered Mental Health in Pediatric Primary Care.” Participants participate in a a 3-day long intensive training in diagnosing and treating pediatric depression, anxiety, and ADHD, with some training on psychosis, oppositional and conduct disorders, and bipolar disorder. This is followed by a six-month, case-based distance learning program. More information on this training can be found at this website:
-
UC Irvine/UC Davis Train New Trainers Primary Care Psychiatry Fellowship
- Interprofessional year-long clinical education certificate program. Primarily focused on adult mental health issues; Longitudinal, one-year learning module.
Mental Health Integrated Care and Telepsychiatry
Effective management of mental health conditions in primary care often involves changing your practice organization in order to offer patients effective prevention, management and referrals. Many of our Chapter members have incorporated integrated care or collaborative care into their practices in order to make their offices and systems of care more aligned with the needs and expectation of patients and families.
Steps to Accomplishing Mental Health Integration
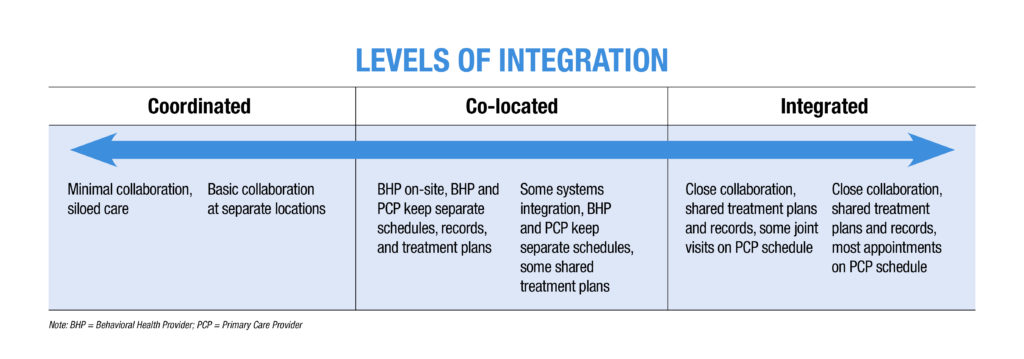
-
Integrating Mental Health and Pediatric Primary Care
- The Center of Excellence for Integrated Health Solutions has a number of excellent videos on Assessing Organization Readiness, Building the Business Case and Workforce Development in building an integrated behavioral health system into your practice.
-
Practice Readiness Inventory
- The purpose of this tool is to help primary care clinicians assess the extent to which their office systems promote and support mental health practice. Use this link to create action items within your practice to improve your mental health readiness.
-
American Psychiatric Association Materials for Integrated Care
- The American Psychiatric Association (APA) has some nice resources on integrated care that is arranged in a user-friendly way. You can explore the articles and videos in the “learn” and “get trained” sections of the American Psychiatric Association (APA) site below.
- Particularly of interest is the section on “Getting Paid in the Collaborative Care Model,” which address a general medical audience.
-
The Family Experience with Primary Care Physicians and Staff from NAMI.org
- A helpful “how to guide” for practices to make themselves more aligned with the needs and expectations of patients and families.
-
What is Telepsychiatry?
- New telepsychiatry guidelines allow you to align your practice with mental health professionals or use telepsychiatry methods in your contacts with patients. This is a helpful description of telepsychiatry and its uses.
-
Telepsychiatry in the COVID Era
- Information from the American Psychiatry Association on new guidelines for use of telepsychiatry. There is also a very useful interview with Peter Yellowlees, MD regarding techniques in use of telepsychiatry.
-
Best Practices in Delivering Virtual Counseling
- This PowerPoint presentation from materials developed by the Mental Health Services Oversight & Accountability Commission (MHSOAC) giveskeys to successful tele-mental health, including worksheets for families, handouts and interactive games.

Explore other sections:
or go back to Mental Health Issue Page
Connect With Your Community

Resources for your patients who need mental health services:
Sources of Specialty Services for Children with Mental Health Problems and Their Families
- While this link is general in nature, it could be used with the Mental Health Practice Readiness Inventory to begin to improve the “navigation” process on getting access to mental health resources
Health Insurance Services
Note that due to Federal Mental Health Parity Laws, all health insurance is responsible for providing mental health services
-
Medi-Cal
Each county has contracted MediCal Managed Care entities, and most of them have subcontracted (e.g. Beacon Mental Health) to provide mental health services for “mild to moderate” behavioral health conditions. This includes counseling, diagnostic services, and psychiatric consultation regarding medication. Some counties have developed explicit rules for what is a “mild-moderate” condition by age, and others are less explicit. For all counties, moderate-severe behavioral health conditions are treated by the County Behavioral Health Program. Most managed care organizations also have case managers to assist families with accessing services.
- Contact information for California Medi-Cal Managed Care Plans: https://www.dhcs.ca.gov/individuals/Pages/MMCDHealthPlanDir.aspx
-
Commercial Insurance
All CA commercial insurers must contract for mental health services and maintain an accurate provider list for members. Families should contact member services for assistance. Most insurers also have case managers to assist families with accessing services.
-
Behavioral Emergency Services
All counties have Behavioral Emergency Services, many of which have separate pediatric and adolescent access points. Many counties utilize an ACCESS phone number for this or use 211.org
-
Suicide Hotlines
- Suicide Prevention Lifeline (24/7) 1-800-273-8255
- Spanish Suicide Prevention Line (24/7) 1-888-628-9454
-
County Behavioral Health Services
For all counties, moderate- severe behavioral health conditions are treated by the County Behavioral Health Program. They treat uninsured as well. Many have special programs that have been funded by the Mental Health Services Act (MHSA). Many counties utilize an ACCESS phone number.
- Contact information for your county’s behavioral health services department:
-
School Based Services
-
School Based Health Clinics: Some schools, mostly middle and high schools, have publicly funded School Based Health Clinics, which are often staffed by physicians, nurses and mental health counselors. They generally provide free counseling services during school hours.
- A list of California School Based Health Centers by county and contact information and services offered is available at: https://www.schoolhealthcenters.org/school-health-centers-in-ca/locations/sbhcs-by-county/
- School Based Mental Health Services: Counseling for children and teens with moderate-severe behavioral health concerns can be offered at school sites and funded through the County Behavioral Health Agency. Check with your County Behavioral Health System to determine eligibility for this service.
- School-funded services: Children are eligible for school-funded counseling and support services when it becomes part of a school plan to improve learning. Examples of these plans are:
-
-
-
- Student Success Team (SST) services
- Section 504 services
- Special Education (IEP services)
-
-
-
- Refer families to the school for evaluation regarding eligibility for these services. Information about requesting an initial evaluation for special education services and a sample letter for parents in English and Spanish is available at: https://www.parentcenterhub.org/evaluation-2/
- Preschool/Childcare assessment and intervention programs: The California Department of Education has an assessment and intervention program for children in preschool or childcare with behavioral or developmental problems. Family Resource Centers, First 5 programs and certified preschools initiate the evaluation and refer to appropriate services. Depending upon the results of the assessment, the child may be eligible for behavioral and family-based treatment in the child care or preschool setting.
- For more information:
-
-
Community Non-profit based services
Most County Behavioral Health Programs contract with local community non-profit based services to serve children and adolescents. These non-profit programs also frequently have endowments, grant-based services and sliding scale programs. A list of non-profits serving children in your area can be found on 211.org or through the MHSOAC Program search tool at: http://transparency.mhsoac.ca.gov/searchpage
-
Advocacy Services for Mental Health Needs

Explore other sections:
Improve Your Practice – Mental Health Skills and Practice Management
or go back to Mental Health Issue Page
Advocate, Advocate, Advocate
The AAP Chapter 1 Mental Health Committee began performed a survey of pediatricians in our Chapter in 2018 to determine perceived barriers to access to mental health services for children in their practice. The study results showed that 38% of the pediatricians responding to the survey felt that their patients “seldom” have appropriate access to mental health services and another 49% felt that access was appropriate “some of the time.” The most critical access barriers noted were in the provision of counseling and support for severe mental health conditions. The top 3 barriers to access identified in the survey were:
- The lack of an adequate number of mental health providers with training in children’s mental health services
- Inadequate reimbursement for mental health services
- The difficulties experienced by patients and families in navigating the referral process for mental health services
Action Steps
After receiving the results of the survey, the Committee developed an action plan to improve access and quality of mental health services in Northern and Central California. AAP California has subsequently adopted improvement in mental health services as a major goal of our outreach and advocacy activities. In partnership with the Medical Education committee, we have offered two in-person CME courses on the provision of mental health care in the primary care office which have trained over 200 pediatricians. We have also partnered with the AAP State Governmental Affairs committee and other partners to submit comment letters to the Department of Health Care Services regarding:
- The credentialing of mental health providers serving children and teens
- The use of EPSDT criteria to permit children to receive mental health services without a mental health diagnosis
- Compliance of Medi-Cal plans with timely access to care regulations for children and teens seeking mental health services.
- Compliance of Medi-Cal plans with CMS Parity requirements that mental health services should have equal access as medical services.
- Funding for trauma and developmental screenings.
Many of these communications have resulted in changes in the regulations governing care for children and teens seeking behavioral/mental health services.
Get Involved!
Chapter members are encouraged to join our committee and get involved in future advocacy and educational activities. Our priorities for action at this time are:
- Increasing access to school mental health counseling and supports
- Increasing access to therapists by assuring adequate payment and health plan/health insurance accountability for services
Please contact Diane Dooley, MD, FAAP at or contact AAP Chapter 1 for more information on joining our committee.
Explore other sections:
Improve Your Practice – Mental Health Skills and Practice Management
or go back to Mental Health Issue Page
AAP Immigrant Child Health Resources
AAP Resources, Policy Statements, Toolkit and Educational Material
The Border is Everywhere
Proactive Tips for Care of Immigrant Kids